Abstract
Background About 20% of patients with venous thromboembolism (VTE) have concomitant cancer. The aim of this analysis is to describe the clinical features, management and short-term course in patients with acute pulmonary embolism (PE) included in the COPE Registry, by cancer status.
Methods COPE is a prospective, multicentre study of adult patients with acute, symptomatic, objectively diagnosed PE. Patients were classified into three groups by cancer status: with active cancer, with history of cancer or without cancer. Active cancer was defined in case of diagnosis performed in the 6 months before study inclusion, metastatic disease or ongoing anticancer treatment. Patients with data unavailable on presence/absence of cancer were excluded from this analysis.
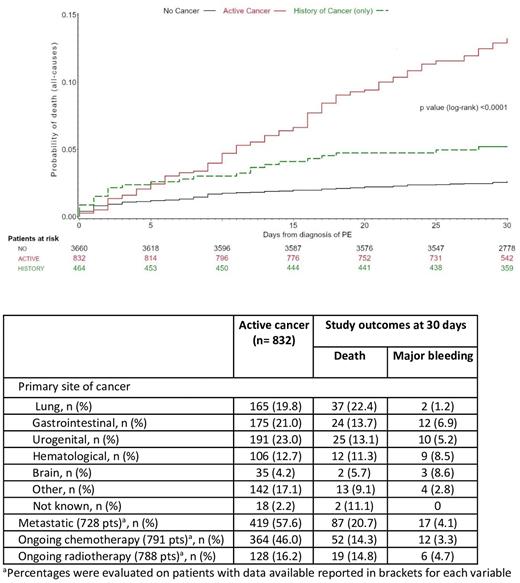
Results Data on cancer were available in 4956 COPE patients (95.1%); 832 (16.8%), 464 (9.4%) and 3660 (73.8%) patients were classified as having active cancer, history of cancer or no cancer, respectively. Among patients with active cancer, urogenital, gastrointestinal and lung cancer were the most common, accounting for about 20% each; at diagnosis of PE, 419 patients (57.6%) had metastatic disease, 364 (46.0%) and 128 (16.2%) were receiving anticancer agents or radiotherapy. Different prevalence of comorbidities and risk factors for PE was observed among patients with active cancer, history of cancer or no cancer. At discharge, a DOAC was given in 43.1%, 78.8% and 82.0% of patients with active cancer, history of cancer and no cancer, respectively. Despite the proportion of high and intermediate-high risk patients was similar, death in-hospital and at 30 days were higher in patients with active cancer compared to patients with history of cancer and no cancer (7.9 vs 4.3 vs 2.2% and 13.8 vs 5.2 vs 2.6%, respectively) (Figure). Similar findings were observed concerning the incidence of major bleeding. In patients with active cancer, death at 30 days was more frequent in those with lung cancer or metastatic disease and major bleeding in those with gastrointestinal, hematological or brain cancer (Table). Among patients with active cancer, death due to cancer, PE or major bleeding occurred in 28, 18 and 5 during the hospital stay and in 66, 19 and 6 at 30 days. The analysis for predictors of death at 30 days in patients with and without active cancer will be available for presentation by the ASH Congress 2022.
Conclusions Among patients with acute PE, those with active cancer, history of cancer and no cancer have peculiar features, different risk for death or major bleeding in hospital and at 30 days. Our findings may challenge clinical practice and inform future studies.
Disclosures
Becattini:Bayer AG: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; BMS: Consultancy, Honoraria; Daiichi Sankyo: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal